Health + Medicine
Artificial Intelligence Takes on Health Care at Hadassah

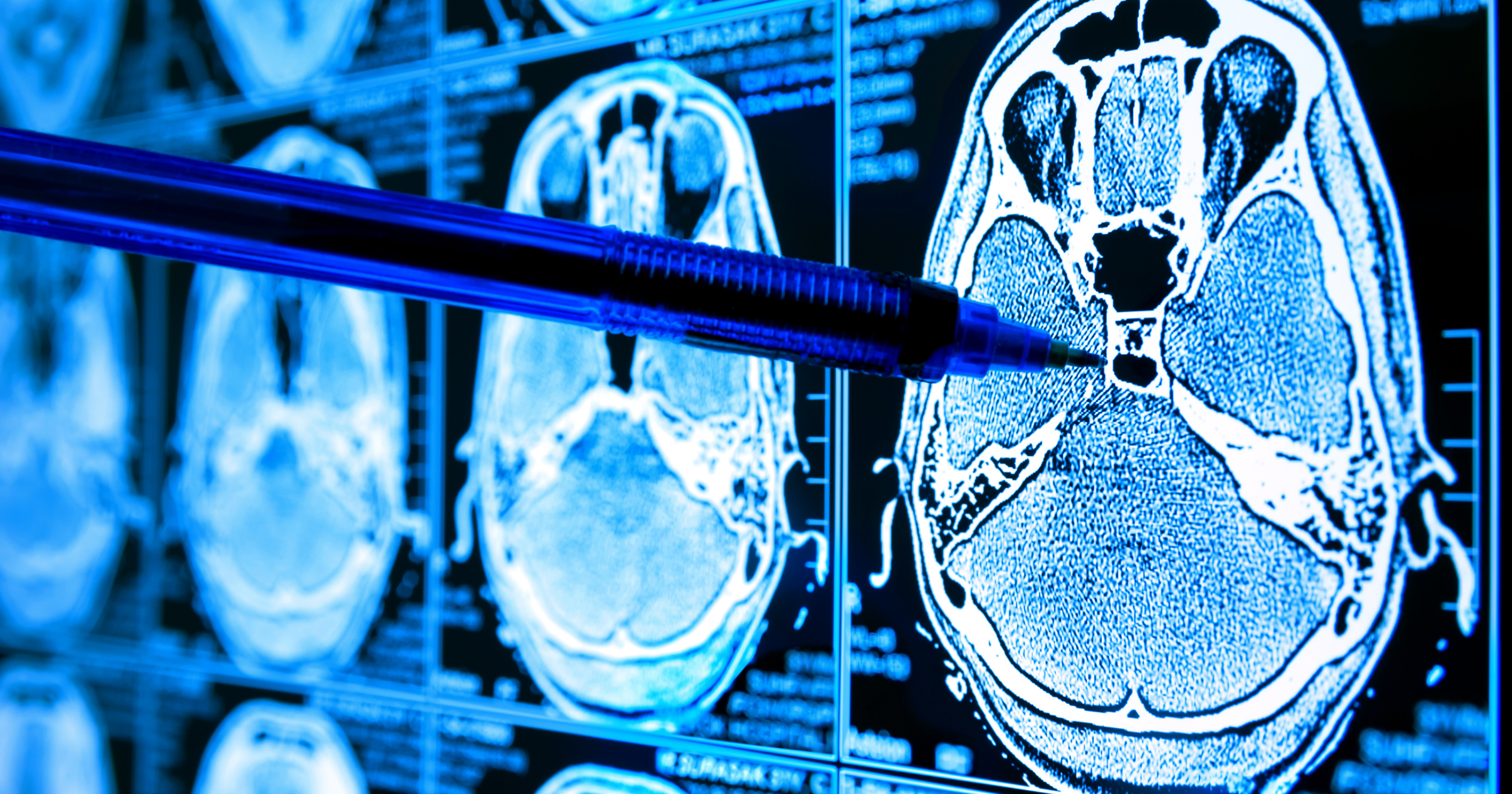
A 43-year-old woman hurries into Hadassah Hospital Ein Kerem in Jerusalem late one Thursday afternoon. Her cancer in remission, she has come for a routine follow-up CT scan and is blindsided when the radiologist sends her to the emergency room. It has nothing to do with cancer, he tells her. The artificial intelligence (AI) software that evaluated her scan has flagged a life-threatening blood clot in her lung.
“With Israel winding down for its weekend, it’s unlikely a radiologist would have read the scan until the following week, a potentially critical delay,” said Dr. Jacob Sosna, chair of radiology and nuclear medicine at Ein Kerem. “Fortunately, our AI tool detected the pulmonary embolism, staff was immediately notified, and she was hospitalized and successfully catheterized” to remove the clot.
This patient, who asked that her name not be used, is one of some 30,000 individuals whose medical images are analyzed by AI servers at the Hadassah Medical Organization each month—and among the 10 percent in whom a clinical concern is identified.
AI, which generally means any human-like behavior displayed or conducted by technology or a machine, has made headlines as a driver of both innovation and transformative change across many fields. In health care, AI is defined as the use of machine learning—computational models that use algorithms and vast amounts of data to recognize patterns—to assist and improve patient experience and streamline research and diagnosis.
Hadassah is gaining renown for its research and use of the technology in a broad array of fields, from oncology to women’s health. Amid the groundbreaking work are a number of AI-focused startups developed by Hadassah doctors that are beginning to transform medicine. In 2025, Newsweek ranked HMO as one of the world’s top smart hospital centers—the fourth year it has received the accolade. Newsweek’s latest ranking of 2,400 hospitals in 30 countries also named Hadassah as one of the best medical centers worldwide.
While many AI innovations are still in their infancy, and much of their use at Hadassah is still in the research phase, the radiology department is one area where AI already is making a significant and practical impact.
“Radiology is technology driven, and it’s pioneering AI in medicine,” said Dr. Sosna, a key figure in the adoption of AI in the department.
Integrating AI into radiology—like integrating it into every other medical and nonmedical field—requires a significant shift. Radiologists are experts in anatomy, pathology and image interpretation but not necessarily in data science or machine learning, so time and training are needed to interpret AI-generated findings. At the same time, AI rollout in hospitals is costly and innovative, so it varies widely across hospitals.
Three-quarters of the more than 1,000 AI medical applications approved by the U.S. Food and Drug Administration are in radiology, with 15 of them used at Hadassah, Dr. Sosna said, “putting us ahead of many academic hospitals in the United States and Europe.”
For radiologists, he explained, “AI is a super-smart assistant. It finds patterns, analyzes floods of data and detects early signs of disease.
“I believe AI tools will be used routinely to predict and prevent disease—screening for osteoporosis, cardiovascular disease, diabetes, genetic mutations and more, long before clinical symptoms appear.”

In addition to scanning patients, the technology will also personalize medical care. “Treatment is traditionally based on what works for the majority,” Dr. Sosna explained. “This saves countless lives, but doesn’t reflect the genetic, biological and environmental differences that make each patient unique. AI does this, enabling highly personalized care plans.”
It also has the potential to transform oncology. Working together with Hebrew University computer scientist Leo Joskowicz, Dr. Sosna is developing an AI-based tool that monitors and analyzes tissue changes in cancer patients by comparing their data across multiple scans. When it was tested on a 52-year-old man with neuroendocrine tumors where no changes were visible to the human eye, AI detected an increase in the number and size of his cancer lesions.
“This told us he wasn’t responding to treatment,” Dr. Sosna explained, “and his therapy was changed.”
The two men are aiming to commercialize this tool, called HighRAD, through their startup of the same name. The tool was developed through Hadasit, Hadassah’s technology transfer and innovation arm.
Beyond radiology, AI technology is poised to revolutionize diagnosis and treatment throughout HMO. Neuro-oncologist Dr. Shai Rosenberg, who heads AI development in the oncology unit, is another key player.
As a young man, he pursued both his love for math and physics and his medical vocation. He completed medical school while creating his own math-physics-computer science program at the Technion’s Excellence Program, then earned a Ph.D. in statistical genetics and performed postdoctoral work in computational biology. Now a senior physician and researcher at HMO, he said that he teaches digital medicine and computational medicine to the Hadassah-Hebrew University medical faculty so that physicians “understand the language of math and computer science.”
Dr. Rosenberg is also co-founder and chief scientific officer of Geno-Cure.AI, a startup built on his cutting-edge research. Together with Hadassah oncologist Dr. Adar Yaacov, Dr. Rosenberg has developed an AI tool for precision oncology—an approach that tailors cancer treatment to the specific characteristics of each patient’s tumor. Named MESiCA, the tool profiles a tumor’s genetics by identifying the unique mutations in a patient’s DNA that triggered the growth of cancer cells. By interpreting these mutations as molecular fingerprints or unique signatures, MESiCA helps reveal the underlying mechanism of the disease and guides personalized treatment.
Hadassah on Call
Decode today’s developments in health and medicine, from new treatments to tips on staying healthy, with the Hadassah On Call: New Frontiers in Medicine podcast. In each episode, journalist Maayan Hoffman, a third-generation Hadassah member, interviews one of the Hadassah Medical Organization’s top doctors, nurses or medical innovators.
In July, Hoffman discussed PTSD with Shiri Ben David, chief psychologist at HMO, and in August, she will highlight the Gandel Rehabilitation Center in a talk with Dr. Elior Moreh, head of HMO’s department of physical medicine and rehabilitation. Subscribe and share your comments at hadassah.org/hadassahoncall or wherever you listen to podcasts.
“Detecting these signatures traditionally requires expensive, time-consuming, whole genome sequencing,” Dr. Rosenberg said. “MESiCA identifies them from a subset of genes, enabling patients to be tested locally without advanced lab facilities.”
All HMO oncology patients now have their genomes sequenced using MESiCA as part of a study in collaboration with Swiss health care giant Roche. Hadassah’s medical center is one of just five worldwide participating in this study, its contribution led by Sharett Oncology Institute head Dr. Aron Popovtzer and medical faculty dean Dr. Eli Pikarsky.
Although still in the research phase, patients from the United States and Israel already turn to Dr. Rosenberg to identify the genetic signatures of their tumors. He hopes MESiCA will soon be more widely available.
AI is also being leveraged at Hadassah in reproductive medicine, such as in vitro fertilization. “It’s bringing new hope to the IVF journey, boosting precision, personalizing treatment and transforming trial and error into data-driven insight and smart prediction,” said Dr. Assaf Ben Meir, director of the fertility and IVF unit at Hadassah Ein Kerem.
With IVF success influenced by a range of factors—maternal age, ovarian reserve, male fertility, egg and sperm quality and embryo development—it can be difficult to pinpoint a cause when it fails. In 2016, Dr. Ben Meir, along with HMO and Hebrew University colleagues, began investigating AI’s potential to improve embryo selection before implantation in the mother. Within five years, they had developed an AI-powered embryo grading platform called CHLOE (Cultivating Human Life through Optimal Embryos), which predicts successful implantation 10 percent more accurately than expert embryologists—and does so hundreds of times faster.
This is the basis of their startup, Fairtility, which has successfully marketed its technology to a host of fertility clinics in Turkey, Spain, Greece and other parts of Europe as well as in the United States. (CHLOE is not used in Israel as IVF is publicly funded and the AI tool uses costly, cloud-based data.) Fairtility’s latest development is applying AI to the soaring demand for oocyte cryopreservation, or egg freezing, particularly in the West.
“Previously, we could assess only whether an egg was ready for fertilization, not its quality,” said Dr. Ben Meir. “We now image oocytes before freezing, using AI to evaluate the potential of what is preserved.”
While Dr. Ben Meir uses AI to support conception, HMO obstetrician Dr. Simcha Yagel, past head of obstetrics and gynecology, harnesses it in research to guide safer deliveries. “In a major hospital like Hadassah, prediction is a large part of what we want to accomplish with AI,” he said. “We’re developing AI tools to integrate into real-world obstetric care to improve outcomes and enhance a woman’s birth experience.”
With ob-gyn colleagues Dr. Yishai Sompolinsky and nurse researcher Michal Lipschuetz, Dr. Yagel is gathering data from thousands of past births at HMO. “We’re collecting information about the mother’s age, ethnicity, demographic background, general health and parity,” he explained. “We also track pelvic measurements, lab results, vital signs, ultrasound data, labor progression, delivery type and complications, and use all this to train AI models to predict the course and outcome of labor and delivery.”
The project has another two years to run, but early results leave the researchers confident of its success. “We expect hospitals everywhere will find it useful for triaging high-risk patients, guiding mother and baby protocols, and improving satisfaction and safety for everyone involved,” Dr. Yagel said.
Heart patients in Israel may also soon benefit from AI. In collaboration with Hadasit, global telemedicine leader SHL Telemedicine and the Hebrew University, HMO cardiologists are developing a tool to detect cardiac risk markers invisible to the human eye, identifying at-risk patients within milliseconds. “This will be a tool that every ECG clinic can use to detect life-threatening cardiac events before they occur and enable fast, potentially critical care,” said Dr. Yitschak Biton, a senior cardiologist at HMO.
With all this, Hadassah is still at the start of its AI journey. Actively fostering its use in health care, the medical center has for the past seven years welcomed digital health startups into its clinics, wards, laboratories and operating rooms as part of the unique Hadassah Startups Program. Established by HMO and run by Hadasit in collaboration with IBM Alpha Zone, it is driving a wave of AI-powered innovations across medicine.
“One of our startups is Olive Diagnostics, which has pioneered a sensor for your home toilet seat that picks up anything from urinary tract infection to prostate cancer, kidney disease and heart disease,” said Masha Zavin, director of marketing, R&D and data collaborations at Hadasit. “Another is Tongo, which enables people who can’t use their hands to control phones, keyboards and other digital devices with their tongues. PathKeeper Surgical, another great example, has developed super accurate real-time optical navigation technology to help spinal surgeons operate more accurately and safely.”
These AI startups are among more than 30 that are alumni of the first digital health accelerator ever established at an Israeli hospital.
“Hadassah’s clinical expertise combines with IBM’s worldclass AI in a 20-week incubator program in which early stage startups develop and test biotechnology solutions in real hospital settings,” Zavin explained. Operating from Hadassah’s BioHouse—a collaborative workspace for biomedical startups initiated at the Ein Kerem campus in 2018—Zavin said that fledgling enterprises are “paired with clinical mentors, advised by IBM, hosted on its cloud and have access to legal, financial, regulatory and marketing advice, without strings, equity or payment…. The program’s 34 graduate companies have realized some $90 million, and a third have agreements with us.”
Many in the field agree that employing AI in health care is likely one of history’s greatest medical advances, on par with vaccines, germ theory, medical imaging, antibiotics and immuno- and stem-cell therapies.
Said Dr. Sosna, “it will become a core part of the digital health system, shaping and supporting modern medicine, transforming health care by earlier and more accurate diagnoses and more targeted therapy, driving breakthroughs and augmenting and amplifying human intelligence.”
Does this mean that our future health care will rest with robotic computers? “Not at all!” Dr. Sosna said. “Health care is a human interaction. You trust your doctor, not your computer. AI is a tool that will help physicians, not make them disappear.”
Wendy Elliman is a British-born science writer who has lived in Israel for more than five decades.







 Facebook
Facebook Instagram
Instagram Twitter
Twitter
Leave a Reply