Hadassah
Health + Medicine
Jewish Women Are Leading the Menopause Movement

As she entered midlife a few decades ago, Beth Segal, a Portland, Ore.-based filmmaker, started noticing alarming symptoms, like pain in her hip joints and heart palpitations. “Completely freaking out,” as she recalls, Segal met with doctors and physical therapists. “Everybody gave me exercises to do,” she says. “But no one once mentioned menopause.”
In fact, until recently, outside of select doctors’ offices, few practitioners mentioned menopause much at all.
The hormonal journey through perimenopause, the prelude to menopause, affects half the population at some point in their lives, often causing hot flashes, sleeplessness, mood swings, brain fog, sexual dysfunction and other symptoms. Yet the major biological transition from perimenopause to menopause to post-reproductive life is scarcely included in most medical training—even for gynecologists.
So it’s hardly surprising that neither Segal nor her practitioners connected her complaints to what used to be referred to discreetly as “the change of life.”
But now that Generation X, 45- to 60-year-olds, has hit midlife, suddenly menopause is everywhere—on television, on social media, on the minds of influencers and in a profusion of wellness offerings.
At the same time, menopause is having a watershed moment in medical innovation and research, with a flurry of new treatments, near-daily headlines about research innovations and a growing consensus that the physical woes of female midlife require more attention. Research also has validated the modern re-embrace of hormone therapy (HT), often considered the most effective way to treat menopausal symptoms.
The cultural and medical momentum is all aimed at a cohort that famously questions authority.
Women in Generation X are “much more likely to advocate for themselves,” opines Dr. Elissa Hellman, an Israel-based, American-born gynecologist who treats patients both in Israel as well as in the United States via telehealth. This is in contrast to their Silent Generation and Boomer mothers, who were more likely to accept whatever their doctors told them—or didn’t tell them—and largely suffered the discomforts of menopause in silence.
“We have seen this explosion of ‘I’m not happy with what they’re telling me because I’m still feeling miserable, so I’m going to do my own research,’ ” Dr. Hellman says.
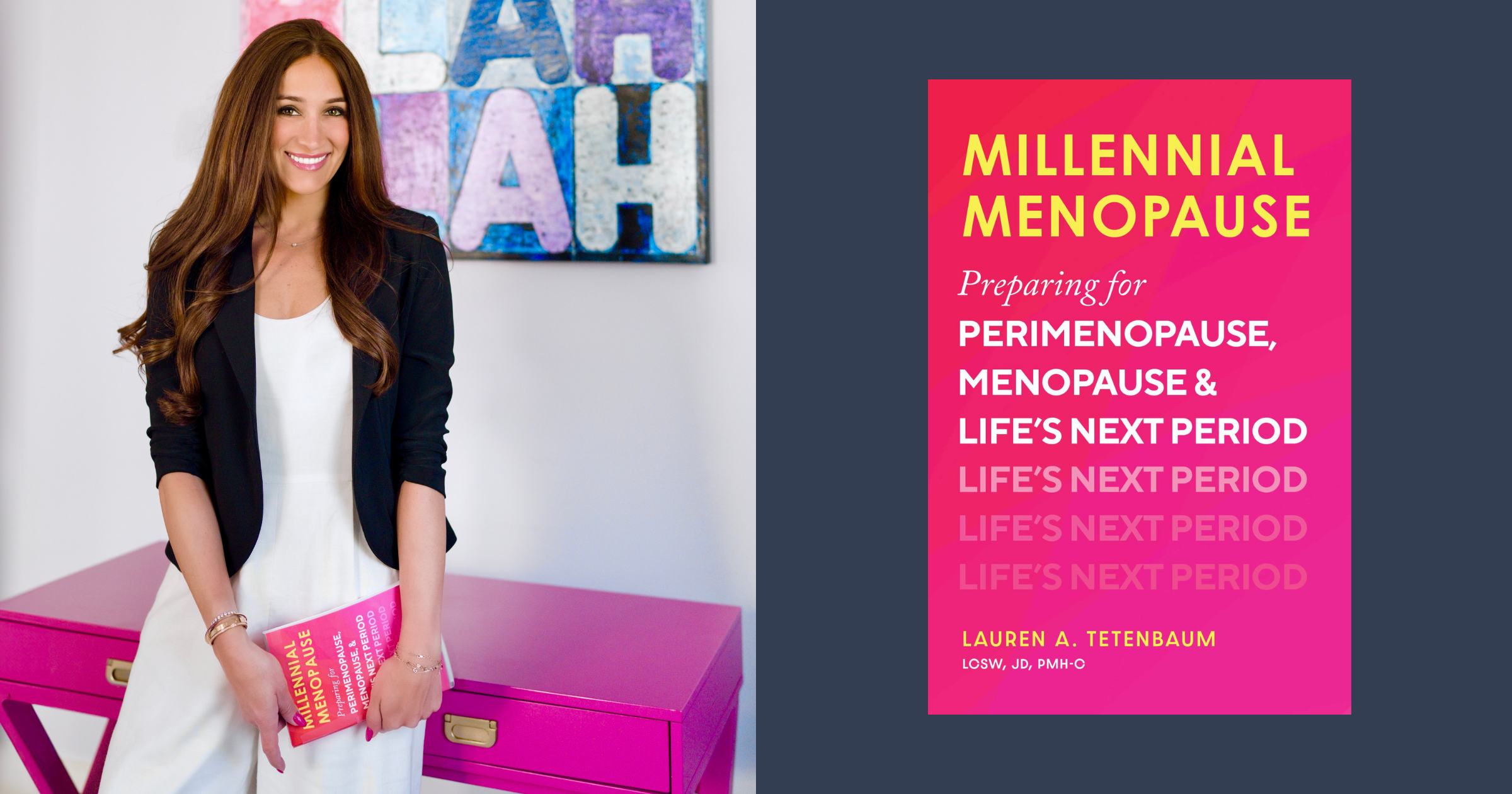
Younger women are raising their voices, too. Millennials “have the opportunity to be proactive instead of retroactive about our health at midlife,” says Lauren Tetenbaum, a 40-year-old psychotherapist and author of the recently published Millennial Menopause: Preparing for Perimenopause, Menopause, and Life’s Next Period.
Fluent in the world of social media, “we are generally more comfortable than prior generations with talking about tough topics—fertility, mental health,” adds Tetenbaum, whose telehealth sessions and workshops promote the holistic and frank approach to midlife outlined in her book. “Menopause is natural, and I believe we all benefit when it becomes destigmatized.”
Jewish women are at the forefront of this menopause movement, prominent not only in the cultural sphere but also in gynecological medicine and research.
In addition to Segal and Tetenbaum, this cohort includes figures such as Joanna Strober, co-founder and CEO of Midi Health; Jennifer Weiss-Wolf, an attorney and feminist activist who co-authored The Citizens’ Guide to Menopause Advocacy; Dr. Mimi Zieman, an Atlanta gynecologist, writer and speaker and the playwright behind The Post-Roe Monologues; and Sheryl Kingsberg, a clinical psychologist and past president of the Menopause Society, a leading nonprofit that provides resources around women’s health in midlife. The organization also licenses health care professionals—including obstetricians and gynecologists, nurses and therapists—to become Menopause Society certified practitioners.
Menopause, which ushers in the post-reproductive life stage for a woman, is defined by a year without menstruation, which, in America, according to the National Institute on Aging, occurs on average at age 52. The postmenopausal stage begins right after that year.
Perimenopause—a clinical term that only recently entered the everyday lexicon—denotes the roughly five-to-10-year phase immediately preceding menopause, in which the body prepares for the end of ovulation. Nevertheless, many use the term “menopause” to refer more broadly to the entire transition from perimenopause to postmenopause.
For Segal—at 60, a member of Generation X—clarity about her symptoms came only when she was recruited to work on The M Factor: Shredding the Silence on Menopause, a 2024 documentary that investigates the impact of menopause on women’s lives that was shown on PBS and at film festivals nationwide. Working on the film, Segal says, helped put her own experience into context—and with its popularity, the documentary became part of a broader conversation.
Witness Oprah Winfrey in her 2025 special The Menopause Revolution chatting up actor Naomi Watts about perimenopausal symptoms and confessing that heart flutters had the legendary talk show host worried she was dying.
And menopause went viral on social media a few months ago with a Saturday Night Live skit, “Emo Mom,” in which Amy Poehler showcased midlife womanhood in a sketch about a cranky mom. Snapping at her teenagers, switching ably into her professional voice when she gets a work call, then venting about her faulty pelvic floor, Poehler nailed the emotional roller coaster that has been compared to a second puberty.
Actor and lifestyle guru Gwyneth Paltrow also has opened up on her Goop website about her own sweating and mood swings and how menopause needs “rebranding.”
New research and interest in HT have also been game-changers. The practice was known for years as hormone replacement therapy (HRT), a term now being phased out in favor of HT or Menopausal Hormone Therapy (MHT). The focus today is on easing symptoms with hormones rather than explicitly replacing what’s been lost.
In a nod to years of advocacy from patients and medical organizations as well as recent findings highlighting the safety and efficacy of novel formulations of hormones, the United States Food and Drug Administration last July removed the black-box warning that had for decades been mandatory on estrogen-containing menopause products. Today, women can opt for estrogen-only or estrogen-and-progesterone pills, sprays or patches as a way of reducing their risk for a number of age-related diseases. There are also lower-dose patches, to treat systemic issues like hot flashes, and estrogen creams and suppositories to aid localized concerns like vaginal dryness and even aging skin.
Women no longer even need an in-person doctor’s visit to obtain these treatments. An empowered generation is driving the growth of online outfits like Midi, a digital medical platform, that are disrupting the traditional medical establishment by catering specifically to women’s midlife needs.
“A lot of women don’t understand that they can feel great, that they don’t have to suffer, that they can thrive as they are aging,” says Strober, Midi CEO, summing up her company’s mantra.
She attributes this misunderstanding to the fertility-oriented focus of most American ob-gyns. With changing guidelines for the frequency and necessity of pap smears after menopause, “most women, after they are done having children, don’t go every year to their gynecologist,” Strober notes. Even if they do, she adds, “Should you wait till your annual appointment to talk about painful sex?”
Midi helps fill that gap, accepting most health insurance for its online appointments with a team of 400 health care practitioners, including ob-gyns, nurses and nurse-midwives scattered around the country and trained in midlife needs. Midi, which Strober co-founded in 2021 with high-tech executive Sharon Meers, now treats more than 200,000 patients nationally, most between the ages of 45 and 55.
Hadassah Magazine Presents
Menopause: New Truths, Old Myths
Join us on January 29 at 7 PM ET for a panel discussion on the changing conversation, latest health trends and medical protocols around menopause. Panelists will include health-tech entrepreneur Joanna Strober, co-founder and CEO of Midi Health; Lauren Tetenbaum, a psychotherapist and author of the new book Millennial Menopause: Preparing for Perimenopause, Menopause, and Life’s Next Period; and Sheryl Kingsberg, head of the behavioral medicine division at University Hospitals Cleveland Medical Center and former president of the Menopause Society. Register here.
Menopause garnered significant attention from American medical researchers in the 1990s with the start of the Women’s Health Initiative, an ongoing, large-scale study into preventing diseases in postmenopausal women. Sponsored by the United States National Heart, Lung, and Blood Institute, it included the largest randomized controlled trial of HT. The initial cohort of women experimented with estrogen and progesterone to ease their hot flashes. However, the study was abruptly halted in 2002 when researchers observed that the women receiving hormones had higher incidences of breast cancer and stroke.
Doctors stopped prescribing hormones “because of the fear of getting sued, of doing harm to their patients,” recalls Dr. David Shveiky, director of the Department of Obstetrics and Gynecology at the Hadassah Medical Organization in Jerusalem. “But biology did not change. Patients suffered.”
Every menopause expert interviewed for this story cited the WHI research as a deeply flawed yet profoundly influential project that essentially scared an entire generation of women and doctors away from treating menopause with hormones.
“We are now, in 2025, mostly digging ourselves out of a huge misstep from 2000—one that led to decades of neglect,” says Weiss-Wolf, the attorney whose new book, When in Menopause: A User’s Manual and Citizen’s Guide, is due out in October.
Multiple articles published in JAMA and other medical journals describe the flaws in the 1990s study, including that the average age of the subjects was 63, a good decade past when women commonly, and more safely, begin HT. They also note the difference between the higher-dose hormones of the 1990s, made from the urine of pregnant mares, and today’s lower-dose, synthetic formulations.
“People need to understand that evidence accrues over time and science evolves, so what’s true today may be contradicted tomorrow,” Dr. Zieman, the Atlanta gynecologist and writer, says. “At any given moment, clinicians are trying to do their best with the evidence they have.”
That’s been the case at Northwell Health in New York, where a cohort of physicians, including ob-gyns, recently completed training and certification by the Menopause Society. Among the ob-gyns was Dr. Valerie Altmann, who hails the movement to revisit menopause treatment—especially now that she is prescribing hormone relief to many of the patients she shepherded through childbirth 15 years ago.
“When you really look at the literature and the research that [the WHI] did, it really was not as bad as the press made it sound,” she says, while acknowledging the study’s flaws. “So there’s been a whole pushback. Women’s quality of life is very important.” The doctor, who lives in Riverdale, N.Y., regularly speaks about menopause to Jewish women’s groups and has appeared on the Jewish Orthodox Women’s Medical Association’s podcast.
The emphasis on quality of life is a longtime focus of Sheryl Kingsberg, both as a clinician-professor and as past president of the Menopause Society and of the International Society for the Study of Women’s Sexual Health. Kingsberg heads the behavioral medicine division and co-directs the Sexual Medicine and Vulvovaginal Health Program at University Hospitals Cleveland Medical Center. She treats her patients with what she calls “a biopsychosocial approach,” including cognitive behavioral therapy, and works closely with physicians on complementary HT.
In particular, Kingsberg is an ardent proponent of long-term, prophylactic postmenopausal treatment with topical vaginal estrogen as a shield against what is now called genitourinary syndrome of menopause. The condition, which affects most women, causes drying and thinning of the vaginal tissues due to a drop in estrogen; the result is painful sexual intercourse and increased incidence of urinary tract infections.
“It’s important for women in menopause to know that this is something that should be addressed and treated,” Kingsberg says. “If their clinician is not talking to them about it, find another one.”
There is broad consensus—backed by research from the National Institutes of Health (NIH)—around the low risks associated with vaginally applied estrogen. For HT overall, however, clinicians acknowledge that the exact portrait of risk versus benefit remains somewhat opaque, depending on the patient’s health profile, dosage, age at onset of treatment and method of administration—which is why all the clinicians interviewed for this story emphasized individualized treatment.
There is, for instance, solid NIH evidence linking HT to a reduced risk for osteoporosis. HMO’s Dr. Shveiky was among those interviewed who pointed out that even if there is a slightly elevated risk for breast cancer, the far greater odds of death from a late-in-life broken hip than from post-menopausal breast cancer might tilt the scales in favor of HT for many women.
In addition, the American Medical Association cites research showing that estrogen therapy can reduce the risks for developing both Type 2 diabetes and cardiovascular disease—the latter of which remains the top killer of women.
According to the Menopause Society, the increased risk for blood clots that can accompany HT might be mitigated by opting for a transdermal patch versus oral treatment. Ways to mitigate breast cancer risk include curtailing the number of years on HT to less than three to five years or starting therapy at a younger age, within 10 years of perimenopause onset.
For Ashkenazi Jewish women—genetically more likely to carry BRCA mutations that significantly raise the risk of hormone-sensitive breast, ovarian and pancreatic cancers—both preventive and post-diagnostic treatments often lead to early menopause and questions about the necessity and safety of HT. The physicians interviewed for this article affirm that BRCA-positive women, including some cancer survivors, may safely use certain hormonal combinations, though in these cases, too, an individualized discussion of risks and benefits is essential.
Then there’s testosterone, the male hormone that also drops, in both men and women, in midlife. The hormone is now being touted as a remedy for flagging postmenopausal libido, but clinicians caution that solid data is not yet available on its risk profile. Kingsberg, who has researched testosterone therapy, notes that the topical gel is still only prescribed off-label to women in the United States. She advises women suffering from hypoactive desire disorder, a persistent lack of sexual desire, to find a clinician skilled in titrating female dosages.
Testosterone is on the menu at Midi, along with GLP-1s for weight loss and what Strober calls “an entire apothecary” of medications and supplements to treat complaints ranging from hot flashes to low energy.

Strober reflects that as a Jewish woman, the Midi mission is especially personal: Many of her clients, like her own family, carry BRCA mutations and, as a result of either breast cancer or ovarian-removal surgery, go into early menopause. “And if they are not given estrogen immediately, their bones deteriorate,” Strober says. “Their sexual health deteriorates.”
“Two million women enter menopause every year, and two million more enter perimenopause. That’s a lot of women,” says Jacoba Atlas, the Emmy Award- and Peabody Award-winning director of The M Factor and its forthcoming prequel about perimenopause, The M Factor 2: Before the Pause. “So all this conversation—it’s only the starting point.”
Dr. Zieman cites a 2023 survey of American ob-gyn residency programs, published in the Menopause journal, that found only 31 percent include a menopause curriculum. “Part of the frustration women have with not getting adequate treatment is because even medical schools and residencies are not paying enough attention to this topic,” she says.
The statistics cited in The M Factor drive home the fallout of this neglect: Of $5 billion allotted by the NIH in 2023 for women’s health research, the film notes that only $15 million went to study menopause. Meanwhile, an estimated 20 percent of the American workforce reports being impacted by menopausal symptoms, and 85 percent of women surveyed in a Mayo Clinic study from 2023 said debilitating symptoms go unaddressed.
The dismissive attitude toward women’s health isn’t limited to the United States. In Israel, Dr. Shveiky, ob-gyn department director at HMO, faced disbelief from colleagues when he chose to specialize in pelvic floor dysfunction, which typically affects women in the second half of life as aging connective tissues weaken, affecting urination and sexual function. Most of his peers were more interested in the higher-profile arena of fertility medicine.
But procedures like in vitro fertilization, while important, are a relatively niche experience, Dr. Shveiky points out, “whereas pelvic floor issues will affect about 50 percent of women in their lifetime,” with the physical stress of childbirth a significant contributing factor. “That’s every second woman. I’m not sure that the training for treating every second woman is less important.”
It’s no coincidence that the majority of menopause-related resources have passionately motivated women behind them. Segal, the filmmaker, describes what she calls the “shocking” lack of interest in The M Factor from virtually any man she talked to about it. “It was unbelievably hard to get funding,” she recalls.
Eventually, Atlas, Segal and their other colleagues recruited a female-heavy sponsorship team that included producer Denise Pines, co-founder of Women in the Room Productions. Pines is also the co-founder of WisePause Wellness, an annual virtual summit on menopause.
Atlas, the director, credits her own decision to start HT during the production of the documentary with “completely turning around” her life. Her previous films—including Birthing Justice, about Black women’s struggle for health equity—lean heavily into social advocacy, a spirit she brought to The M Factor.
She is proud to be among a cohort of Jewish women shattering yet another barrier. “I think my niece, who’s in her early 40s, will have a very different experience with menopause,” Atlas says. “And that’s a good thing.”
Hilary Danailova writes about travel, culture, politics and lifestyle for numerous publications.







 Facebook
Facebook Instagram
Instagram Twitter
Twitter
Ronda Einbinder says
Osteoporosis needs to be discussed and women need Dexa scans much earlier than recommended.
Rachel Goodman says
It’s very surprising that Dr. Rachel Ruben wasn’t discussed. She should have been mentioned in this article – she was one of the doctors who advocated at the FDA to get the black box warning removed from estrogen and was also involved getting the GSM guidelines updated and spread the word about it.
Theresa Linsner says
Agree! Dr. Rubin is excellent
Susanna Levin says
I highly recommend The Menopause Manifesto by Dr. Jen Gunter (she also has a substack), a no-nonsense expert in the field who has all the latest research at her tips. This enables her to give good information straight up, as well as take down the ‘influencers’ who spew half-truths and nonsense.
Yael Pipano Peer says
Thank you, toda!!!
Shirley segal says
I read the articulation on menopause today in haddasah magazine with much interest.
I am 98 yrs old now have my own history on such matters , and think I might have some interesting data to contribute .
If interested please contact.
Shirley segal